 6th Jul 2015
6th Jul 2015
Effective Treatments for Frozen Shoulder
Frozen shoulder sounds like an urban myth but it is a very real and treatable condition in physical therapy. The onset of frozen shoulder in patients can be spontaneous and unknown in origin; however there are groups at higher risk for developing it. Those with diabetes, post-surgery who have long periods of inactivity with their shoulders, and women over 40 are at risk. And fun fact; frozen shoulder won’t likely recur in the same shoulder, but can switch sides. Not so fun, is the fact it can take 1-3 years to recover.
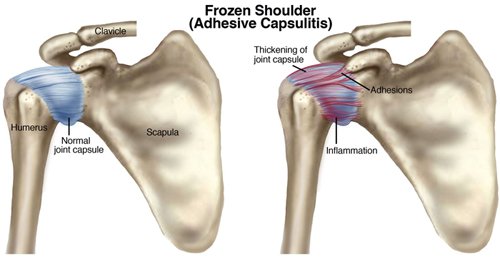
What is Frozen Shoulder (Adhesive Capsulitis)?
Adhesive capsulitis is the stiffening of the shoulder due to scar tissue. Frozen shoulder causes your shoulder joint capsule to shrink, which leads to pain and reduced range of shoulder movement. Your shoulder capsule is the deepest layer of soft tissue around your shoulder joint, and plays a major role in keeping your humerus (arm bone) in the shoulder socket.
What are Frozen Shoulder Symptoms?
Stage 1 - "Pre-Freezing"
During this stage, it may be difficult to identify your problem as adhesive capsulitis. There is pain with active movement and passive motion (movements that a physical therapist does for the patient). The shoulder usually aches, but pain increases and becomes "sharp" with movement. There is a mild reduction in motion during this period, and the patient will protect the shoulder by using it less. The movement loss is most noticeable in "external rotation" (when the arm is rotated away from the body), but a patient might start to lose motion when they raise their arm (called "flexion and abduction") or reach behind them (called "internal rotation"). They will have pain during the day and at night.
Stage 2 – "Freezing"
By this stage, patients have had symptoms for 3 to 9 months, most likely with a progressive loss of shoulder movement and an increase in pain (especially at night). The shoulder still has some range of movement, but this is limited by both pain and stiffness.
Stage 3 – "Frozen"
Symptoms have persisted for 9 to 14 months, and there is greatly decreased range of shoulder movement. During the early part of this stage, there is still a substantial amount of pain. Toward the end of this stage, however, pain decreases, with the pain usually occurring only when a patient moves the shoulder as far as they can.
Stage 4 – "Thawing"
Symptoms have now occurred for 12-15 months, and there is a big decrease in pain, especially at night. Patient’s still have a limited range of movement, but their ability to complete daily activities involving overhead motion is improving at a rapid rate.
Frozen Shoulder Treatment
Physical therapy is the best way to treat frozen shoulder. A physical therapist's overall goal is to restore movement so that a patient can perform all their daily activities. Once the evaluation process has identified the stage of the condition, the physical therapist will create an exercise program tailored to each patient’s needs. Exercise has been found to be most effective for those who are in stage 2 or higher.
Stages 1 and 2
The physical therapist will help maintain as much range of motion as possible and will help reduce the pain. A
physical therapist will use a combination of stretching and manual therapy techniques (massage, ultrasound machines, electrical stimulation) to increase range of motion. Heat and ice might be used to help relax the muscles prior to other forms of treatment. Also, the therapist will create an at-home exercise program designed to help reduce the loss of motion.
Stage 3
The focus of treatment will be on the return of motion, with the therapist using more aggressive stretching, joint mobilizations and manual therapy techniques (massage, ultrasound, e-stim). The patient may begin some strengthening exercises as well, and their at- home exercise program will change to include these exercises.
Stage 4
In the final stage, the therapist will focus on the return of "normal" shoulder body mechanics and the patient’s return to normal, everyday, pain-free activities. The therapist will continue to use stretching, strength training, and a variety of manual therapy techniques.
Sometimes, conservative care cannot reduce the pain. If this happens, the physical therapist may refer the patient for an injection of anti-inflammatory and pain-relieving medication into the joint space. Research has shown that although these injections don’t provide longer-term benefit for range of motion and don’t shorten the duration of the condition, they do offer short-term benefit in reducing pain.
With origins unknown and length of recovery so long, it’s important for patients to seek treatment to keep them active in their daily lives. Driving, working at the computer, picking up the groceries, there aren’t many activities that don’t incorporate shoulder movement. The patient’s instinct may be to keep the shoulder immobile to avoid the pain, but you can see by the treatment plan the opposite is true. Manual therapy with modalities and exercise are the most effective way to treat the very real occurrence of frozen shoulder.
For more physical therapy resources and devices see ProHealthcareProducts.com






