 22nd Apr 2022
22nd Apr 2022
THERAPEUTIC ULTRASOUND - A Comprehensive Guide
Therapeutic ultrasound: A Compliment to Musculoskeletal Rehabilitation
(Therapeutic Exercise, Mobilization + Ultrasound)
THERAPEUTIC ULTRASOUND
Therapeutic ultrasound produces acoustic vibrations of high frequency (not detectable by human ear) that produce thermal and/or nonthermal effects in the body’s tissues.
Unique advantages over other nonacoustic heating modalities:
- Sound waves selectively heat tissues high in collagen(e.g.,tendons, ligaments, muscles, joint capsules, menisci, nerve roots, periosteum, and cortical bone) without causing a significant tissue temperature increase in skin or fat.
- Provides therapeutic benefits by stimulating normal body physiological functions to perform better for the primary purposes of enhanced soft tissue injury repair and pain relief.
- Greater tissue heating depth penetration: For example: a 4-minute whirlpool@105ºF (40.6°C) produces a temperature increase at 1cm below the fat tissue of about 2.0°F(1.1ºC).At the same 1cm depth,3 MHz ultrasound treatment increases temperature over 10.8°F(6°C).
THE ULTRASOUND UNIT: 4 MAIN PARTS
- Generator: a high frequency electric generator linked through an oscillator circuit and a transformer. Control panel: on-off, power, time, intensity, duty cycle, continuous or pulsed modes, 1 or 3MHz frequency, and automatic shut-off in case the crystal overheats.
- Crystal: a thin synthetic ceramic crystal that is a transducer that convert selectric energy to acoustic energy through mechanical deformation (expands&contracts) of the crystal that causes the soundhead to vibrate resulting in the mechanical production of high-frequency sound waves.
- Soundhead: a ceramic, aluminum, or stainless steel plate attached to the crystal that is a transmitter that transfers the acoustic sound waves from the crystal to the tissues where it causes the tissues to vibrate.
- Applicator: this is the housing for the crystal and the soundhead. A handheld device that facilitates the application of the ultrasound to patients. It should be ergonomically designed so that when held the wrist is able to be kept in a neutral position where it is functional strong to withstand the constant motion required to apply the therapy without succumbing to a repetitive motion injury.
HOW DOES ULTRASOUND WORK –THE PHYSICS
Sound
Sound is created when a force acts upon a molecule causing it to vibrate back and forth which then sets in motion a cascade of molecular vibrations producing a mechanical wave (soundwave).
- Ultrasound is a mechanical wave in which energy is passed by the vibrations of the molecules of a biological medium through which the wave is traveling, concentrating the energy in a targeted or limited area.
Types of sound waves
- Longitudinal waves: these waves travel with vibration (molecular displacement) in alignment or longitudinally through soft tissues.
- Transversewaves: these waves vibrate in a direction perpendicular to the longitudinal waves, such as when the sound wave rebounds after hitting bone.
Frequency of sound wave transmission
In body tissues, the higher the frequency of sound wave, the greater the amount of ultrasound energy that is absorbed in the tissues, resulting in less energy that is transmitted to deeper tissues.
- 3MHz frequency–these sound waves are absorbed superficially and are only transmitted to a depth of 2-3 cm.
- 1MHz frequency–these sound waves are transmitted deeper before being absorbed to a depth of approx.6 cm.
Attenuation
Attenuation is a decrease in energy as a sound wave passes through body tissues as some of the energy is
absorbed in the tissues.
- Fat tissue: minimal energy absorption
- Muscle tissue: has a high rate of energy transmission
- Dense tissue high in protein: energy is well absorbed in this type of tissue
- Tissue high in water content: the energy penetrates easily to a deeper level
- Superficial bone: energy is easily absorbed
- Peripheral nerves: energy is absorbed at a rate twice that of muscle
Characteristics of crystal – also impacts how well ultrasound will penetrate tissues.
The quality of a crystal can affect how well the ultrasound wave penetrates tissues.Crystal
quality is partly determined by:
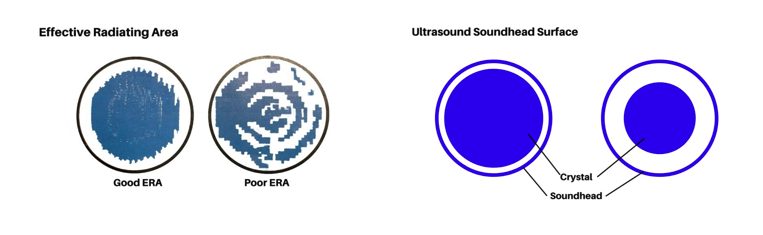
- Effective Radiating Area (ERA): The surface area of a soundhead that transmits a sound wave from the crystal to the tissues.
- Beam Nonuniformity Ratio (BNR): A measure of the uniformity of the ultrasound beam.
EFFECTIVE RADIATING AREA (ERA)
ERA is the surface area of a soundhead (faceplate) that transmits a sound wave from the crystal to the tissues. Important considerations include:
- The ERA is always smaller than the crystal and sometimes significantly smaller than the soundhead.
- The entire surface of the soundhead does not radiate ultrasound output.
- It is recommended that the total size of the crystal and soundhead surface match as closely as possible for ease of application in order to maintain the most effective contact with the targeted tissue area.
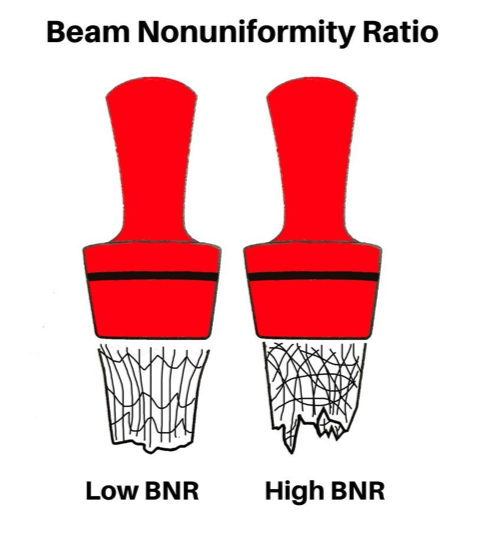
BEAM NONUNIFORMITYRATIO (BNR)
The BNR is an indicator as to variability of intensity with in an ultrasound beam as they are not completely uniform–with some point higher and other points of lower intensity. The BNR is the ratio of the spatial peak intensity (highest intensity in the beam), to the spatial average intensity (average intensity across the beam).
- A good BNR is between 2 to 5. The lower the BNR, the more uniform the ultrasound output will be and the less likelihood of developing hotspots.
- HotSpot: An area at tissue interfaces that may become over heated from too much concentrated energy in one area, resulting in discomfort and potential tissue damage.
- The higher the BNR ratio, the more important it is to use lower intensities or move the soundhead faster during treatment to avoid hot spots.
ULTRASOUND TREATMENT PARAMETERS
The“therapeutic dose” of ultrasound is determined by these parameters:
- Mode
- Frequency
- Intensity
- Treatment Length
- Treatment Area Size
ULTRASOUND PARAMETER - MODE
Ultrasound devices produce “continuous” or “pulsed” mode ultrasound.
- Continuous Mode: the ultrasound energy remains constant (100%) throughout the treatment.
- Pulsed Mode: the ultrasound energy is periodically interrupted so that no ultrasound energy is being produced during the “off” period.
- Duty Cycle: the percentage of time that ultrasound is generated over one pulse period.
•Pulse Duration (on time) x 100/Pulse Period (on-time+off-time)
•Example: pulse duration of 10ms & total pulse period of 40ms. The duty cycle would be 25%= the total amount of energy delivered to the tissues would be only 25% (10x100=1,000/40=25).This means that the total amount of energy delivered to the tissues would be only 25% of the energy delivered if a continuous mode was used.
ULTRASOUND PARAMETER - FREQUENCY
Therapeutic ultrasound typically has a frequency range of 0.75 to 3.0 MHz.
Ultrasound frequency determines the depth of tissue penetration and the rate of tissue heating.
- 3 MHz frequency sound waves are absorbed more superficially (2cm - 3cm depth) and therefore are best for treating conditions that are more superficial. For example, medial and lateral epicondylitis, patellar tendinitis, plantar fasciitis, Achilles tendinitis, radial or ulnar nerve entrapment, hand/finger and foot/toe joints, carpal tunnel syndrome, muscles close to the body surface, etc.
•At 3 MHz the rate of absorption/attenuation is not only absorbed more superficially but is also absorbed 3 times faster than at 1MHz and therefore heats the tissue 3 times faster.
- 1 MHz frequency sound waves are transmitted through the more superficial tissues and absorbed primarily in deeper tissues (3cm to 6cm depth). Because of its depth of penetration, it is recommended to use this frequency on individuals with a high percentage of body fat and when deeper tissues need to be heated.For example, deeper muscles such as piriformis, soleus, hip internal rotators, supraspinatus, or larger joints, etc.
ULTRASOUND PARAMETER - INTENSITY
Intensity is the rate at which energy is being delivered per unit area and is a function of both the pulse width and pulse frequency, measured in watts (W). Also referred to as spatial average intensity (SAI). SAI is the intensity of the ultrasound beam averaged over the area of the soundhead.
- SAI= Total watts(W) / Effective radiating area(cm²)=W/cm².
- There are no definitive guidelines for intensity for selecting specific ultrasound intensities during treatment. A safe range of intensity for a moving soundhead is 0.5to3W/cm².
Thermal ultrasound treatments should feels lightly warm and adjusted to patient tolerance. If there is a significant adjustment in intensity it should be countered with an adjustment in the treatment time.If intensity is increased, treatment time is reduced. If intensity is reduced, treatment time is increased.
ULTRASOUND PARAMETER – TREATMENT LENGTH
The length of treatment time for any individual should be based on:
- Size of the area to be treated should only be about 2x to 3x the size of the soundhead, otherwise the energy will be distributed too broadly, and therapeutic temperature will not be reached
- Ultrasound frequency (remember, ultrasound at 3MHz heats tissues 3x faster than1MHz)
- Intensity in W/cm² (the lower the intensity the longer the treatment time)
- Desired temperature increase
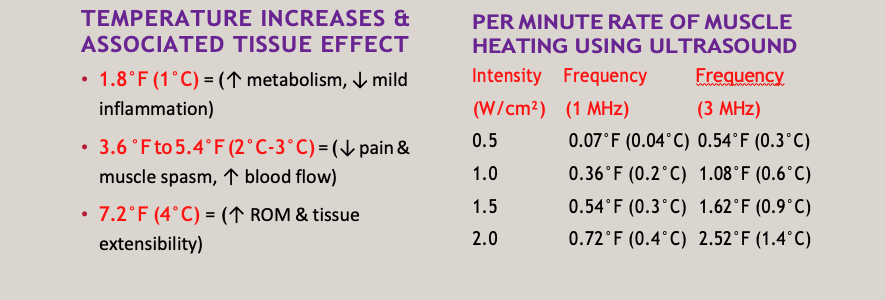
DETERMINING ULTRASOUND TREATMENT LENGTH–THE “GUESSTIMATE” METHOD
- Scenario:Patient is experiencing medial epicondylitis. In preparation for massage and eccentric resistance exercises, you want to heat the origin of the wrist flexor muscle group. An appropriate approach would be to:
- Heat the muscle tendon junction using 3MHz frequency at an intensity of 1W/cm². This would take approx. 7minutes to reach the 7.2°F(4°C) temperature.
•1W=1.08°F(0.6°C)/minx7minutes=7.6°For4.2°C
Note: If at some point the patient complains that the temperature is too hot and uncomfortable, simply decrease the intensity dose and add some additional treatment time.
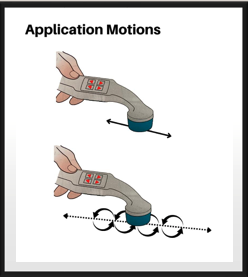
TREATMENT AREA SIZE & SOUNDHEAD MOTION
- Treatment Area Size: Ultrasound is a very effective tool for heating deep tissues. However, the treatment should be limited to an area that is two or three times the size of the ERA of the crystal, or twice the size of the soundhead surface to ensure proper heating depth.
- SoundheadMotions: Ultrasoundhead can be moved in back-and-forth linear strokes or small over lapping circular motions at a rate of 3-4cm/second.
ULTRASOUND BEAM TRANSMISSION–THE MEDIUM OF “GEL”
Ultrasound beams must be transmitted from the soundhead to the patient through a coupling medium, either a gel or emersion in water. The coupling gel serves as a lubricant and fills incongruities between the soundhead and skin, helping to ensure that the ultrasonic energy enters the target tissue at the desired intensity. Important considerations include:
- The application of gel to the body surface treatment area should be sufficient in amount to maintain good contact and lubrication, but not allow air pockets to form from the movement of the soundhead.
- When administering the treatment with a gel medium it is essential that the soundhead’s surfacere main in complete contact with the body surface at all times. Lifting or tilting the soundhead at an angle of even 15° will result in a significant reflection loss of energy and reduced treatment effects.
- Ultrasound gel should be stored at temperatures above 104°F(40°C) to prevent bacterial growth on the gel bottle tips.
ULTRASOUND BEAM TRANSMISSION – “IMMERSION OF THE SOUNDHEAD IN WATER”
- The container of the water should NOT be metal as this will reflect some of the ultrasound.
- The water used for immersion should be at least body core temperature, not room temperature, to ensure the desired “thermal” effects.
- The soundhead should move parallel to the body treatment surface area at a distance of less than1cm.
- If air bubbles form on the soundhead or treatment area, wipe them off immediately.
“THERMAL” EFFECTS OF THERAPEUTIC ULTRASOUND
- Increased local blood flow–delivering oxygen and nutrition to healing tissues
- Increased extensibility of connective tissues (tendons, joint capsule, adhesions, scar tissue) enhancing the effectiveness of stretching
- Increased metabolism in tissues in which heat is absorbed
- Diminished pain perception – increased blood flow that washes away metabolic waste products/chemical irritants that cause pain
THERAPEUTIC ULTRASOUND –AS AN AID TO “STRETCHING CONNECTIVE TISSUE”
Just as plastic is hard and not pliable when cool, connective tissues have a some what similar characteristic. However, heat up the plastic object and it becomes pliable and can be stretched. Heat up connective tissues and they become more pliable and extensible and can more effectively be stretched/elongated.Therefore, to enhance the effectiveness of stretching, joint mobilizations, friction massage, muscle warm-up, you should stretch these tissues when they are still warmed, preferably immediately after ultrasound treatment is terminated. The window of opportunity for this therapeutic benefit is around 5 to10 minutes.
“NONTHERMAL” EFFECTS OF THERAPEUTIC ULTRASOUND
- Tissue regeneration
- Facilitating inflammation and wound healing
- Cell membrane alteration – facilitating diffusion of metabolites and promoting protein and collagen synthesis
- Increased phagocytic activity of macrophages
“INDICATIONS” FOR USE OF THERAPEUTIC ULTRASOUND
- Soft Tissue Shortening – restoring ROM lost from contracture and/or scare tissue – combined with stretching when tissue is still warmed
- Soft tissue healing and repair
- Diminish pain – increased blood flow that washes away metabolic waste products/chemical irritants that cause pain
- “itis”conditions–tendinitis, bursitis, fasciitis,
- Musculoskeletal syndromes/conditions (carpal tunnel, nerve entrapment, TMJ dysfunction)
- Ligament sprains, muscle/tendon strains
- Trigger points – desensitization
- Muscle spasms – heated tissues have increased blood flow → eliminates chemical irritants, alters nerve conduction speed and relaxes muscle tension (e.g., IT Band tightness)
“CONTRAINDICATIONS” FOR USE OF THERAPEUTIC ULTRASOUND
- Acute and post - acute conditions with continued bleeding
- Over reproductive organs (a gravid uterus) – could potentially damage developing fetus
- Cancer – a local exposure may contribute to metastasizing from increased blood flow
- Over eyes – could cause cavitation in the fluid compartments
- Impaired arterial circulation – sufficiently healthy to meet the increased metabolic demand
- Over spinal cord after laminectomy – cavitation may occur in the cerebrospinal fluid
- Over pacemaker or carotid sinus – could affect normal pacing of heart or baroreceptors
- Thrombophlebitis – potential to cause an emboli
- Presence of infection – heat could accelerate infection
“PRECAUTIONS” FOR USE OFTHERAPEUTIC ULTRASOUND
- Over epiphyses of bones of young children – in high doses may disrupt growth by affecting early closure
- Over metal implants- potential to heat implant
- Over areas of impaired sensory – could hinder patient feedback on excessive heating
- Excessive exposure to bony prominences – to avoid concentration on periosteum
- Only use intensities considered therapeutically safe – to avoid cavitation and the potential for tissue damage
ULTRASOUND &ELECTROTHERAPY
The combination of ultrasound and electrotherapy (combination therapy) involves the stimulation of muscle contraction as the ultrasoundhead serves as an electrode in delivering the electrotherapy. The benefits of combination therapy are:
- Pain reduction and muscle contraction stimulation
- Effective in the treatment of myofascial trigger points
- Effective in reducing the pain-spasm-pain cycle
INSTRUCTIONS FOR USE OF ULTRASOUND – PREPARATION FOR APPLICATION
- Application of ultrasound should be performed using only calibrated and properly working ultrasound unit
- Identify specific location for treatment (may consider marking area so stay within 2x to 3x ERA) and evaluate for any sensory deficit in the skin, for open wounds or rashes
- Explain to patient the procedure – gel medium, sound waves generate gentle warmth, report if any feel of hot, total Tx time, etc
- Prepare patient – positioned and draped for comfort, modesty, and accessibility to treatment site, including positioning for access to deeper tissues
- Use appropriate soundhead size
- Apply appropriate amount of gel medium (or immerse part in tepid water)
INSTRUCTIONS FOR USE OF ULTRASOUND – SET APPLICATION DOSAGE
Frequency: 1MHz for mod to deep tissue penetration “or” 3 MHz for superficial tissue heating
Mode:
- Continuous: the ultrasound energy remains constant (100%) throughout the treatment
- Pulsed: the ultrasound energy is periodically interrupted so that no ultrasound energy is being produced during the“off”period.
•Duty Cycle: the percentage of time that ultrasound is generated over one pulse period
Intensity: The lower the intensity the longer the treatment time. Also, adjust the intensity to the patient’s heat perception. If it gets too hot for the patient, move the applicator faster as you turn down the intensity.
Treatment Duration:
- 1MHz: 10 to15 minutes for vigorous heating
- •3MHz: 3 to 7 minutes for vigorous heating
INSTRUCTIONS FOR USE OF ULTRASOUND – OTHER CONSIDERATIONS
- Frequency of therapy applications: 1x to 2x daily
- Number of treatments: approximately 14 sessions
- If goal is to increase joint ROM, place body part in stretch position during latter part of ultrasound application and stretch the tissue immediately after termination of ultrasound
POST THERAPY PROCEDURES
- Clean the soundhead of gel and disinfect
- Wipe any remaining gel from the patient’s skin
- Performanystretchingormobilizationtechniqueofthepatientwhilethetissueisstill warm and pliable
- Documentation of ultrasound treatment dosages: Frequency, intensity, mode and duty cycle if pulsed, size and location of treatment, treatment length, patient response to treatment, etc.
REFERENCES
- Draper,D.O.,Jutte,L.S.,Knight,K.L.,Therapeutic Modalities: The Art and Science,3rd
Edition
- Cameron,M.H.,Physical Agents in Rehabilitation: From Research to Practice, 4th Edition





